Reflections of a Global Chameleon
How working in different parts of the world influenced my outlook on the most important aspects of life as an ophthalmologist.
At a Glance
- David Almeida spent time in Hungary, Canada and the USA over the course of his varied career
- He compares different types of healthcare systems he’s observed in Europe and in North America and points out their strengths and weaknesses when it comes to treating patients
- David reflects on different attitudes to the right balance between work and life outside of it, and shares the lessons he’s learnt from practicing in different parts of the world.
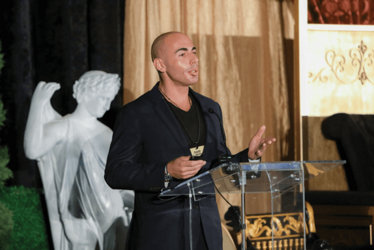
In the course of my career, partly thanks to my background, partly the choices I made, and partly coincidentally, I have had the opportunity to work in different countries on both sides of the Atlantic. In terms of education, I truly feel like a citizen of the world, and my upbringing made it quite easy for me to blend into different environments, almost like a chameleon, as I’m sometimes affectionately referred to by my wife. I often feel the need to move from one country to another and can’t seem to be able to stay in one place for too long.
I was born in Lisbon, Portugal, and moved to Canada when I was eight years old. That’s where I received my education, up to the point of starting my PhD at the University of Toronto. I was focused on drug design and new product development and unexpectedly got a chance to finish my PhD in Szeged, Hungary, a couple of hours south of Budapest. The year spent in Hungary opened my eyes to how colleagues and collaborators from all over the world look at the same problems in unique ways. It really taught me how helpful it is to look at a specific challenge using different points of view.


The experience proved very useful when I returned to Canada to do my medical degree and complete my residency at Queens University in Kingston, Ontario. My thinking process was this: if I’m going to design good drugs and work on the innovative side of product development, I need to learn more about the end users: patients.
I’ve never lost my ability to compare diverse viewpoints and I got another chance to explore different attitudes to healthcare and work-life balance when I moved again to Washington DC. Later, I did my vitreoretinal diseases and surgery fellowship at the University of Iowa and, after a few years in Minnesota, we are very fortunate to call Charlotte, North Carolina, home; this is where I joined a dynamic and growing practice, Metrolina Eye Associates. Through all my travels, with my wonderful wife Jasmine and now our children, I have appreciated the adventures of the past and the growth it has given me on a personal and professional level.
Different folks, different strokes
I’ve had a chance to observe dissimilar healthcare systems in Europe, Canada and the States, and each one has advantages, as well as constraints. During my time in Canada, which has a more socialized healthcare system (largely due to the government being the overwhelmingly dominant single payer), I thought a lot about equal distribution of resources; and how it could serve the greatest number of people. Trying to figure out how best to allocate available funds and give individual patients the best outcomes without paying extra inspired me to do an MBA in healthcare management at The George Washington University School of Business.
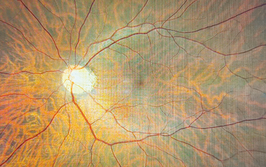
And that really was an eye-opener. I was able to get a great insight into the American healthcare system and compare it with the structures I’d seen in Canada and in Europe. It was surprising to see how within a private system, by definition focused on individuals rather than society as a whole, innovation was at the forefront, with a lot of resources available for research and development. There were so many new projects able to get funds, which I knew from experience was much harder in Canada and in Europe. I was really intrigued. At that point, I got into the vitreoretinal space, and diabetic retinopathy was probably one of the key areas in ophthalmology that needed product development: new drugs for the future.
From the point of view of an ophthalmologist, I can see a difference in how doctors are able to treat patients, depending on the system they are working within. In Canada, there’s a joke: “Everyone has a right to healthcare, and everyone has a right to wait for that healthcare.” In these socialized structures you always have to think about the patient population as a whole, focus on the entire group, rather than the individual. That means that more people are able to receive care, but within the limits set by the system. There is a utilitarian component of working for “the greatest good for the greatest number.”
However, each patient is different, so treating them all as a homogenous group doesn’t always work. And that’s where the American system comes in, focusing on the individual patient and his or her specific needs. This particular point of view is individualistic without being deterministic. There are often more options available in terms of treatment, although you always have to take insurance into consideration. The Canadian approach might have fewer options available, but you know that those options can mostly be used, without discussion, as they have already been approved. In the US system, there is a cost aspect that needs to be taken into consideration and discussed every time. It’s really important to me to make sure that patients know exactly what costs to expect and that we can choose the best solution for each particular situation, based on the available resources. This, for me, is ‘healthcare realism,’ which, I believe, is missing from the serious political debates on healthcare.
Another aspect of the privatized system is that private practices usually have the latest equipment and machines, as there certainly is an element of competition. A practice can’t afford to use old equipment or implement old standards. My multi-specialty practice relies on excellence in care; if we don’t provide the best care with the most up-to-date and evidence-based tools, we cannot achieve that mission statement.
Finding the right balance
Different approaches to treatments are not the only thing I’ve noticed while working in different countries; there is a noticeable disparity when it comes to work-life balance. In Hungary, it seemed that work had to be done, but doctors had a keen sense of consideration for other personal and professional commitment. If we were going to a research meeting, everyone would get the train, which might have taken a bit longer, but we would use the time to prepare our talks or posters. In my opinion, no one works harder than US physicians and doctors due to the demand from the multiple vantage points of healthcare, innovation and economics. Because of this, I see a lot more opportunities for doctors in the States, so it seems like people have more of an incentive to work longer hours. There are certainly more collaborative research projects available, with more funding, which is helped by the size of the population. In my experience, Canada probably falls somewhere in between the European and American attitudes.
I’ve found that Canadian doctors tend to be happier to stay in one location than their American counterparts. Many of my colleagues did their undergraduate and medical studies in Toronto, followed by residency and finally a job in the same place. In the US, people seem to be constantly traveling to different places, often switching states for a year. I never thought I would be doing as much traveling as I do, because my mentors in Canada didn’t seem to move around so much. But I think that the willingness to travel keeps ideas flowing and makes professionals feel more connected. In this regard, I feel more American than European or Canadian.
Ophthalmology around the world
Today, the way that ophthalmic conditions are treated in Europe and North America is becoming increasingly standardized and protocol-driven. One difference that I have noticed is that techniques and instrumentation seem to get adopted much faster in Europe, perhaps thanks to fewer regulatory barriers. I find being able to try new instruments and new approaches to surgical problems very exciting.
I feel that I’ve benefited greatly from having the insights into different healthcare systems and attitudes to providing care. Canada’s more socialized structure taught me to treat every single patient equally, not according to their ability to pay or their socio-economic status. If a person needs to see me, it doesn’t matter whether they have the funds or not; I deal with all the financial issues later. I’m also a minimalist when it comes to resources, which I think is another aspect I picked up while working in Canada. I have learnt to do the most with the tightest resources and I apply it to the way I perform surgery. This, of course, has implications for the final bill presented to the patient and works very well in the American system because of my relative frugality when it comes to extraneous tests and procedures. Make no mistake, this does not mean taking chances or depriving the patient of needed interventions; instead, it means having a strategy to ensure the best care without waste.
My time in Hungary taught me that collaboration – gaining different perspectives – is absolutely crucial to finding good solutions. I’m a co-founder of a pharmaceutical company Citrus Therapeutics and we try to apply this philosophy constantly, working with various people who have different inputs into designing new and better drugs. The cross-pollination of ideas is one of the most rewarding outcomes of collaboration.
Consider the stereotypes: American doctors down a jug of coffee or Red Bull before starting a day at the clinic, because they know they’re going to be working long hours, seeing hundreds of patients; Canadian doctors struggle to work with limited resources, cursing the government that doesn’t spend enough on healthcare or value their role in the delivery of care. There are elements of truth and myth to any stereotype but, in reality, I feel that many cultural generalities break down in the operating room, when it comes to the vitreoretinal ophthalmic space. There we become more alike than we are different, irrespective of geography and habits.