Dual Blade, Single Purpose
Malik Kahook wanted a better way to image the trabecular meshwork in cadaver eyes, and designed and built a blade that was capable of removing tissue strips intact. The Eureka! moment came when he realized it could be used to lower IOP in glaucoma patients too
Where did the idea for the Kahook Dual Blade (KDB) come from?
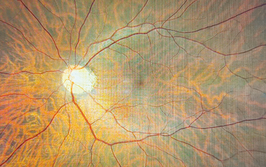
We have a busy translational research program here at the University of Colorado, and one project was imaging the trabecular meshwork (TM). Harvesting the TM from cadaver tissue is difficult – it’s a bit like wet tissue paper, and is hard to remove in one piece in order to perform anatomically correct imaging. This limitation made me take a step back and design a device with the properties I needed.
Around 40 versions came and went before we began honing in on the ramp that exists after the distal-most point of the device, which stretches the tissue and raises it above the normal plane of the TM. We worked hard to find the geometry that functioned best, and then went on to create the blade with help from outside contractors. One day when harvesting tissue, I realized what we had, and said “Wait a second, we could use this to perform goniotomy surgery in patients with glaucoma!” It seems obvious now, but innovation often leads you in a different direction to your original goal.
What motivated you to pursue your idea?
In glaucoma surgery, our gold standard is trabeculectomy; if that fails, we’ll perform tube shunt surgery. These procedures are effective, but they’re associated with adverse events, and since they were introduced, we’ve been trying to improve our toolkit. When I saw how well the KDB worked in cadaver tissue, it was a natural decision to try and use it to improve surgical outcomes in my patients. I thought if we could cleanly remove the TM without leaving significant tissue leaflets behind and open a pathway for fluid to exit the eye, this could have a significant impact on how we address high IOP. And since glaucoma is a disease of the TM, we’re removing the root cause of raised IOP, without disrupting other tissues.
What outcomes have you seen?
We’ve seen a decrease in IOP (around 5 mmHg) for six months in a large cohort of patients, and a significant decrease in the number of topical medications required, with around 70 percent of our patients decreasing their dependence by at least one drug (1–4). New World Medical launched the device in the US last year, and we’re following around 120 patients as part of an initial survey. We’ll soon have one-year data on this group, and right now, all the indications suggest that we’ll see that this 5 mmHg drop is sustained beyond six months.
We’re currently looking at all patient types – those with mild, moderate, or severe disease, and with many different forms of glaucoma – we’re even having great success in very advanced glaucoma cases. Unlike some glaucoma surgeries that are only approved in conjunction with cataract surgery (which can be an obstacle for pseudophakic patients, and create reimbursement issues in the US), we’ve successfully used our device in both phakic and pseudophakic patients. The benefit to the patient is that they can have this procedure done prior to (and hopefully obviating the immediate need for) a trabeculectomy or drainage device. It’s a huge success if we can push away a trabeculectomy or drainage device for a year or two, and even better if we can push it off into the distant future so that we’re not even thinking about it, and I think we’re starting to see that. I’ve seen this robust IOP lowering firsthand in my own patients, and I’ve observed that combining the procedure with cataract extraction adds IOP lowering efficiency, and a more significant drop in medication dependence.
What feedback have you received?
The device has been marketed in the US since November 2015, and is now available in Europe and Canada. My US-based colleagues are seeing the same things – a significant lowering of IOP and a decrease in medications. They’re also using the device in many forms and stages of glaucoma. Some are choosing to use it in combination with cataract surgery, and others are using it on their pseudophakic patients, or even patients who had cataract surgery with a MIGS device in the past, who need their IOP lowered further. I’m seeing a lot of excitement about the variety of patients that the device can be applied to – all without reimbursement concerns. I believe the KDB could become a key tool for glaucoma surgeons – instead of perfecting a large repertoire of procedures to treat glaucoma, the KDB offers surgeons versatility, and great outcomes in a wide range of patients.
- J Kennedy et al, “Initial experience with a novel dual blade device: safety and utility of use”, AGS Annual Meeting, March 2016.
- G Lazcano-Gomez et al, “Novel dual blade device for ab interno trabeculotomy”, AGS Annual Meeting, March 2016.
- S Abdullah et al, “A novel dual blade device for goniotomy: initial clinical experience”, ARVO Annual Meeting, May 2016.
- Data on file with New World Medical