The Art Of Eyes
Popular culture has always viewed eyes as being things of beauty. But there’s more to the eye than the color of your irides. Advances in imaging technology have enabled us to see far more than could ever have been imagined. And on closer inspection they’re still beautiful.

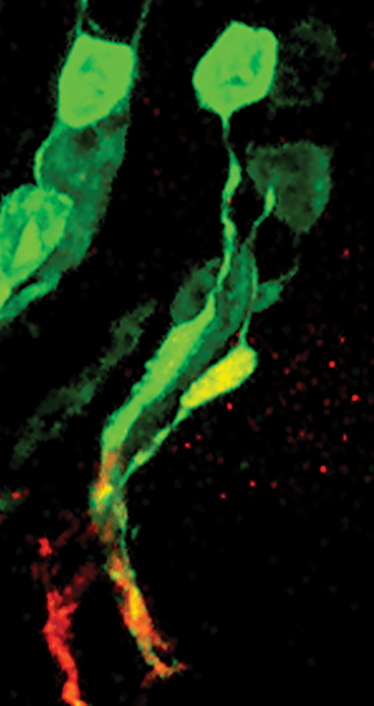
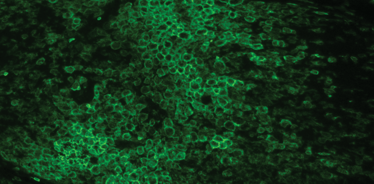
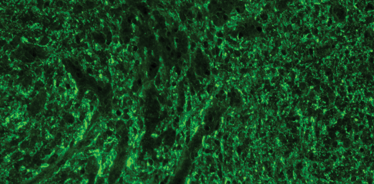
A cluster of nascent retinae generated from 3D embryonic stem cell cultures.
The retinae contain photoreceptor precursors that express normal photoreceptor proteins, including visual pigment. Rhodopsin is labeled green and the phototransduction enzyme, recoverin, is labeled red.
Image by Anai Gonzalez-Cordero, a post-doctoral researcher at University College London, UK.

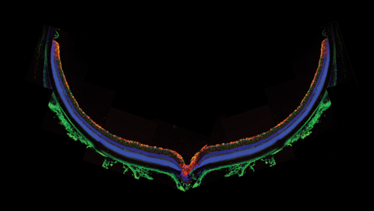
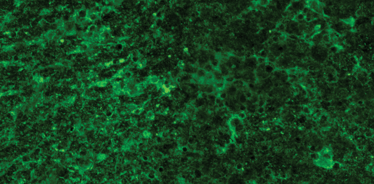
Colorful confocal characterizations
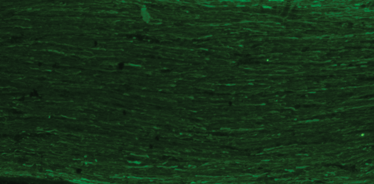
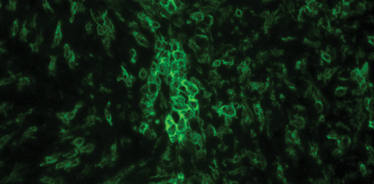
Exploiting the power of confocal microscopy to characterize the retinae of mice.
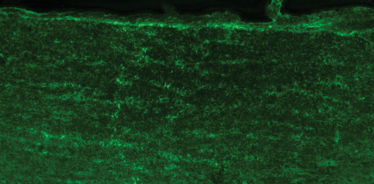
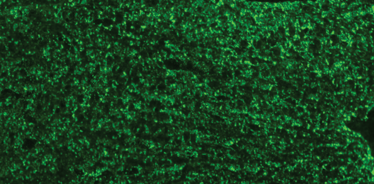
A cross section of an adult wild-type mouse retina immunostained for reactive gliosis markers, showing little in the way of glial reactivity and an orderly retinal architecture.
Amanda Barber is a Sir Henry Wellcome post-doctoral research fellow at the University of Cambridge, UK.

Subretinal signaling secrets
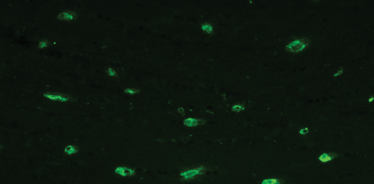
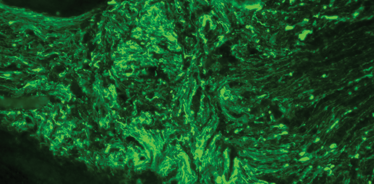
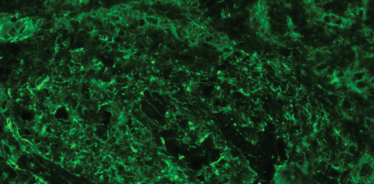
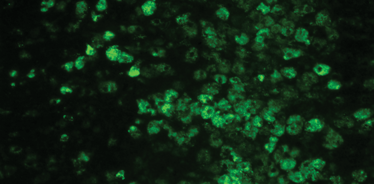
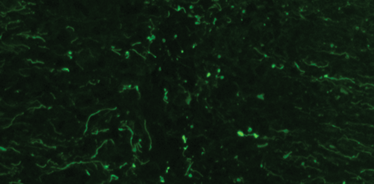
Transplantation studies reveal new aspects of photoreceptor development.
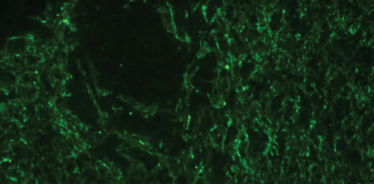
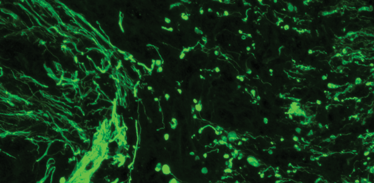
Photoreceptor precursor cells transplanted from 4-day old mouse pups into the retinae of adult mice, do one of two things. Some integrate into the host retina, but others fail to do so and aggregate, forming clusters. Despite failing to integrate, subretinally-located clusters (top) develop outer segments (green), yet their counterparts at the vitreal side of retina (bottom) fail to develop them, indicating that important extracellular signals are present at the subretinal space that allow the final differentiation and maturation of these photoreceptors
Dominic Erbele is a post-doctoral researcher at the Technical University of Dresden, Germany.

Everyday art
A couple of beautiful images from patients presenting to an ophthalmology department in Prague.
Conventional meibography using a transilluminating light probe.
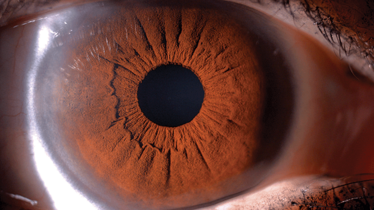
Chocolate cake-like iris.
Bohdan Kousal is a Prague-based medical retina specialist, and a co-founder of the Ophthalmic Genetic Center at the Czech capital city’s Charles University.

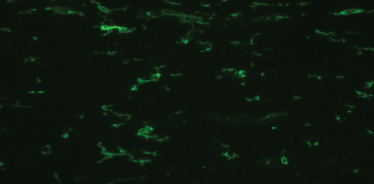
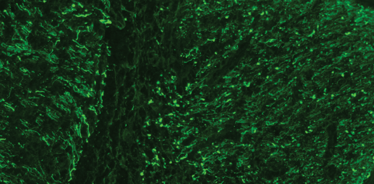
Optic crush aftermath
Immunohistochemical analyses reveal the extent of the damage.
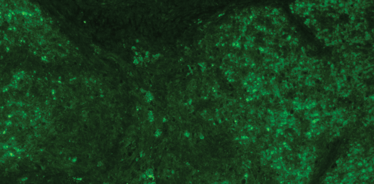
Optic nerve crush (ONC) was performed on deeply anesthetized adult male Wistar rats, using specially-designed cross-action tweezers. Crushes (of uniform intensity) were performed for 30 seconds, and time points from 6 hours to 20 days were investigated via immunohistochemistry.
Sven Schnichels is a Laboratory Head at the University Eye Hospital, Tübingen, Germany.
Untreated (control) optic nerve:


Waiting for the clinic to open
“A blind man is a dead man” – Peruvian proverb.
Fewer than one in five Peruvians have health insurance. Inevitably, many are blinded by age-related eye disease – even relatively easily remedied ones like cataract. Silvia Frilo is an ophthalmologist who treats as many of the poorest in Peruvian society at the CEPRECE clinic in Cusco. This lady is one of his patients, waiting for the clinic to open.
Image provided by Bodo Hufeland of Geuder AG.

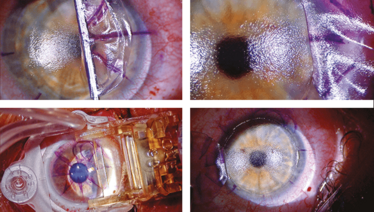
Anatomy of a sub-Bowman’s keratomileusis flap
Femtosecond lasers gather a lot of attention, but it’s worth remembering the advantages of the microkeratome, and what it can achieve.
Here I’ve used an automated blade microkeratome (One Use-Plus, Moria SA, Antony, France) to cut a sub-100 µm flap. The flaps appear smoother and less traumatized than those cut with a femtosecond laser, and since no bubbles are formed, there are no bubble-related issues to worry about, and you don’t run the risk of opaque bubble layer formation, laser-induced light sensitivity, or plasma bubble breakthrough. Non-laser flaps can be lifted without tissue dissection and they do not require hourly steroids to suppress the plasma-induced inflammatory response.
James Lewis is the Director of Cataract, LASIK and Corneal Surgery at the Pennsylvania College of Optometry, Salus University, Elkins Park, PA, US

Heidelberg Engineering stands for excellence in diagnostic imaging. A broad offering of multi-modal imaging devices provides ophthalmologists and optometrists with versatile imaging platforms for daily clinical practice. Early diagnosis and treatment monitoring with Heidelberg Engineering devices allows clinicians to take advantage of advanced therapeutics. With its passion for technology, Heidelberg Engineering is blending the newest research findings with established clinical methods to build devices for daily practice. Through constant innovation the company extends the range of available modules for its future proof expandable platforms. Image data workflow solutions support the easy integration of the broad range of devices.
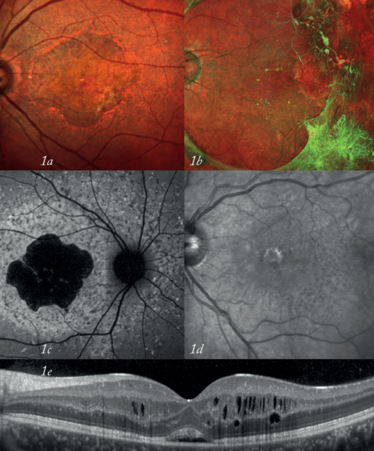
(1) Get the full picture Multi-modality diagnostic imaging (SPECTRALIS®): MultiColor scanning laser imaging
(1a, geographic atrophy; 1b, vitreoretinal traction), BluePeak blue laser autofluorescence (1c, cone-rod dystrophy), IR reflectance imaging (1d, reticular drusen), spectral-domain OCT (1e, cystoid macular edema)
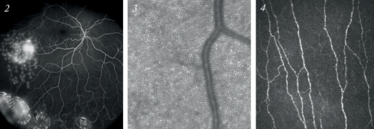
(2) See more Ultra-Widefield FA angiography (SPECTRALIS®): vasculitis (3) See in more detail High-resolution cSLO imaging of photoreceptors (experimental set-up) and (4) confocal microscopy of corneal stromal nerve fibers (HRT Rostock Cornea Module).

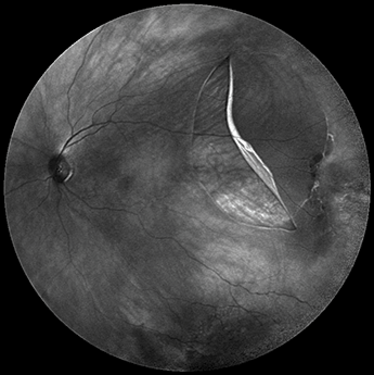
Retinal detachment
An ultra-widefield infrared retinal scan that clearly shows not only the full extent of this patient’s retinal detachment, but also other changes in the inferior and temporal periphery.
Courtesy of Heidelberg Engineering.


Where the cones are kept
The macula lutea and foveal avascular zone captured in fine detail.
Fluorescein angiogram images of a fovea centralis in a depressed area at the center of the macula lutea, measuring about 1.5 mm in diameter. Here, we see a fovea centralis in a depressed area in the center of the macula lutea, measuring about 1.5 mm in diameter.
Filofteia Tacea, an Ophthalmology Fellow, and Richard Hancock, an Ophthalmic Photographer at based at Aintree University Hospital, Liverpool, UK.
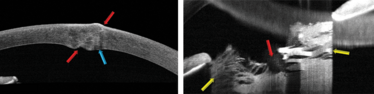
A rose thorn in the lens
A patient was gardening when he was struck by a rose bush branch in his face and eye. Despite having a painful scratchy irritation, he waited several hours to obtain emergency care, and once he did, was immediately referred to an ophthalmologist.
On examination, an obvious impact location on the cornea was observed. When tested, it was Seidel negative, meaning that it was either non-penetrating or self-sealed. An Anterior Chamber SD-OCT test was performed using the Optovie RTVue 100.
Left: The red arrows show the path of the penetrating thorn. The blue arrow shows some of the damage from the trauma.
Right: The rose thorn penetrated the lens (red arrow), and the aqueous humor hydrated the lens, making it "bloom" (yellow arrows). The patient required urgent lens extraction and IOL implantation to restore near normal vision and remove the risk of angle closure.
Image courtesy of Bill Dilworth and Peter Naismith of Optovue Inc., Freemont, CA, USA.

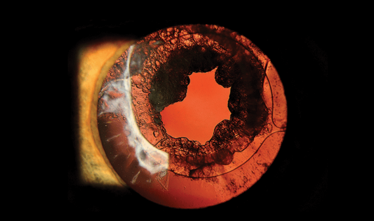
Post-cataract fibrosis
Posterior capsule opacification is caused by the formation of fibrosis on the posterior lens capsule after cataract surgery.
Treatment is by YAG laser capsulotomy, an outpatient procedure in which a laser is used to remove the fibrosis.
Image contributed by Kim Baxter, Ophthalmic Photography Team Leader at Addenbrooke’s Hospital, Cambridge, UK.


Pigment deposits
A moderate slit beam is projected at a 45° angle to the lens pathology – in this case, pigment deposits – and is directly illuminated.
The pupil was dilated to provide the most effective imaging possible.
Image captured by Cees van Beek using the Haag-Streit BX 900.

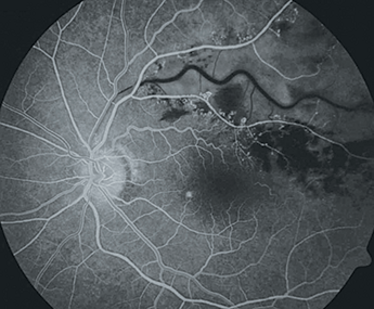
Bravo, BRVO
Common diagnoses can be beautiful.
A 50-year old patient presented with left eye metamorphopsia. His best-corrected visual acuity was 10/10 and fundoscopy revealed a typical supero-temporal branch retinal vein occlusion (BRVO) secondary to thearteriovenous crossing.
Four months after the diagnosis, fluorescein angiography imaging revealed a remarkable BRVO with anatomical characteristics consistent with an ischemic transition.
Image contributed by Inês Martins de Almeida, of the Centro Hospitalar Entre Douro e Vouga (CHEDV), Feira, Portugal.


An incredible CRAO
A magnificent image of a maleficent manifestation.
Central retinal artery occlusion with sparing of the cilioretinal artery territory and whitening of the remaining posterior pole retina in a 47 year-old male with undiagnosed systemic hypertension.
Image contributed by João Pedro Marques, Department of Ophthalmology, Centro Hospitalar e Universitário de Coimbra (CHUC), Coimbra, Portugal.

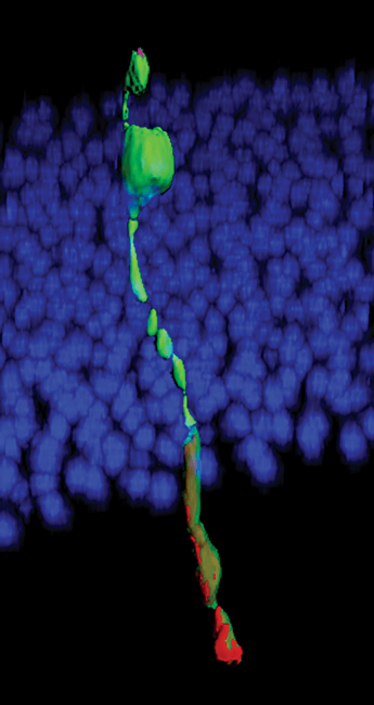
Newly transplanted, but a typical morphology
Three dimensional (3D) reconstruction of a transplanted photoreceptor (green) generated from 3D culture of embryonic stem cells. The newly integrated cell resembles a typical rod photoreceptor.
Image contributed by University College London researcher Colin Chu.

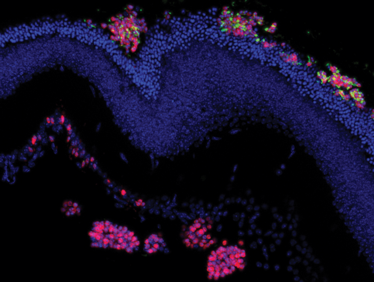
Transplanted photoreceptors
Here, we see the detail of integrated embryonic stem cell-derived photoreceptors following transplantation into a degenerate adult mouse retina. The transplanted photoreceptors express the essential phototransduction enzyme, α-Transducin (red), which is absent in the recipient retina.
Image contributed by University College London researcher Anai Gonzalez-Cordero