Great Minds Look Ahead
The 2018 Power Listers offer a glimpse of ophthalmology’s future
Ophthalmology is an ever-changing field with a pioneering attitude – it’s why so many breakthroughs and innovations in medicine and technology are made in eyecare first. For 2018, we asked the influential leaders making up the Power List for their vision of where ophthalmology is heading.
The future of cornea
“I’m currently trying to solve the surgical challenges in Descemet’s membrane endothelial keratoplasty (DMEK) surgery, which is probably one of our most difficult surgical procedures in corneal transplantation today. The current surgical approach to DMEK makes it generally inappropriate for complex or high-risk cases, where it is needed most – especially as it has the lowest rejection risk. I'm currently evaluating a completely new surgical approach to this procedure.” Donald Tan, Professor at the Singapore National Eye Centre and Duke-National University of Singapore Medical School, Singapore.
“It is exciting to see how the discovery of the pre-Descemet’s layer has evolved into direct clinical applications, both from our own research but more importantly from research by other independent groups around the world. We have made new discoveries in relation to this and other aspects of corneal transplantation, which are either in press or submitted to reputed journals.” Harminder Dua, Head of the Division of Ophthalmology and Visual Sciences, University of Nottingham, Nottingham, UK.
“Corneal transplantation has changed considerably over the last 15 years and many of those changes are thanks to technology derived from refractive surgery! Microkeratomes enabled Descemet’s stripping endothelial keratoplasty (DSAEK), which ended up evolving into DMEK. I expect both procedures will be replaced by therapeutic modalities, such as corneal cell therapies with Rho Kinase inhibitors. Stromal substitutes are already in development and I expect synthetic corneas will become more commonplace. Stem cell treatments will have a role, so long as the correct concoction of cytokines and growth factors can be found to get stem cells recruited from the bone marrow and provide the necessary repairs required.” Sheraz Daya, Medical Director, Centre for Sight, East Grinstead, UK.
“I have been pursuing new modalities for corneal and ocular surface disorders. In the future, I would like to establish cultured corneal endothelial cell injection therapy for bullous keratopathy.” Shigeru Kinoshita, Professor and Chair of Frontier Medical Science and Technology for Ophthalmology, at Kyoto Prefectural University of Medicine, Kyoto, Japan.
“[Ten-year goal:] to develop direct evaluation technology to evaluate corneal biomechanical properties to screen for keratoconus in its earliest manifestations, and predictive models for corneal interventions, such as laser ablation and cross-linking to individualize treatment parameters.” J. Bradley Randleman, Professor of Ophthalmology at the Keck School of Medicine, University of Southern California, and Medical Director of Beverly Hills Clinic, USC Gayle and Edward Roski Eye Institute, Los Angeles, CA, USA.
The future of cataract and refractive surgery
“As a profession, our biggest challenge is the growing backlog of cataract blindness in the developing world. Though our own patients are beneficiaries of increasingly sophisticated technology, cataract blindness will not be solved by refractive IOLs and femtosecond lasers. Different innovations that are low tech, affordable, and more easily mastered than phacoemulsification are needed. Manual small incision cataract surgery (MSICS) is the most important innovation so far. I work with a group within Iantech, which is devoting resources to developing a low-cost iteration of its miLOOP that could be used for MSICS in resource-limited countries. I am also working with a team that is developing a promising topical medication that could prevent or potentially reverse cataract formation. A non-surgical way to halt or delay cataract blindness will have a far wider global impact than any surgical intervention ever could.” David Chang, Clinical Professor, University of California, San Francisco, CA, USA.
“In lens-based procedures, I believe the future lies in the ability to modify the IOL power after implantation, as well as the development of the types of accommodative IOLs. Surgery-wise, the future lies in the field of increased precision of surgical procedures given to us by robotic systems and lasers. As for corneal refractive procedures, I consider refractive index shaping with intra-stromal laser application very promising.” Boris Malyugin, Deputy Director General at S. Fyodorov Eye Microsurgery Institution, Moscow, Russia.
“I believe the future is now, and there are great ideas out there that just have to be filtered and put into clinical practice. The future is what we make out of it, and I believe it is very important that we, as specialists, come together with the industry to design our own future in the best interest of our patients.” Florian Kretz, CEO of Augenärzte Gerl, Kretz & Kollegen; Lead Surgeon, Augentageskliniken Rheine & Greven; Consultant & Research Coordinator of the International Vision Correction Research Center Network (IVCRC.net), University of Heidelberg; and CEO of the NGO Augenärzte für die Welt GmbH, Germany.
“I believe [the future] will be focused on three major areas. One will be for non-accommodative patients where the use of a new generation of IOL will restore accommodation; the lens capsule will be the key to this technology. The second will focus on the younger patient group and include more advanced – and more customized – corneal-based corrections. The third will be for irregular and unstable corneas, for instance with keratoconus, which will likely use tissue addition and in situ molding of the cornea with biomaterials.” Ioannis Pallikaris, Founder and Director of the Institute of Vision and Optics, University of Crete, Greece.
The future of glaucoma
“There’s definitely a tide change. We have so many treatment options (some could say too many at the moment, as we try to make sense of them all!). What I see coming is data increasingly driving our decision making and becoming more integrated; AI-assisted systems pulling together IOP, retinal nerve fiber layer (RNFL)/ ganglion cell layer (GCL) analyses with (better measures of) visual field function and possibly newer variables like outflow resistance, episcleral venous pressure and methods of predicting conjunctival fibrotic response to surgery. We’ll be able to detect smaller rates of change and more accurately predict future risk. With this comes tailored management of need versus risk which is constantly appraised.” Dan Lindfield, Consultant Ophthalmologist and Glaucoma Director, Royal Surrey County Hospital, Guildford, UK.
“We will move to more remote monitoring of care and will increasingly have access to more effective treatments. Blindness rates will be greatly reduced.” David Friedman, Professor and Director of the Dana Center for Preventive Ophthalmology, Wilmer Eye Institute, Johns Hopkins Hospital, Baltimore, MD, USA
“[Future goals:] collaborating with scientists, industry and regulatory agencies to develop the first neuroprotective agent (to protect the optic nerve independent of lowering IOP).” Robert Weinreb, Director of the Shiley Eye Institute and Hamilton Glaucoma Center, University of California, San Diego, CA, USA.
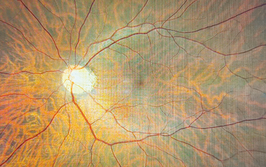
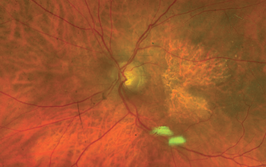
The future of retina
“Breakthroughs in gene and stem cell therapy will provide immense opportunity for advancing medical and surgical approaches to eye disease, and fighting degenerative retinal disease, while big data, telemedicine, and analytical advancements in AI and deep learning will enhance public health and lift our level of evidence-based medicine.” Julia Haller, Ophthalmologist-in-Chief, Wills Eye Hospital; William Tasman Endowed Chair, Professor and Chair of Ophthalmology, Thomas Jefferson University, Philadelphia, PA, USA.
“[The future?] Retinal prosthesis implants with much smaller pixels. Ultimately, we hope to achieve single-cell resolution, which might restore visual acuity at a level better than 20/80. In addition to photovoltaic restoration of sight, we are working on transplantation of photoreceptors, and the results are extremely encouraging!” Daniel Palanker, Professor, Department of Ophthalmology and Director of the Hansen Experimental Physics Laboratory at Stanford University, Stanford, CA, USA.
“Argus II is just the beginning. I hope to restore color vision and enhance reading vision so that patients can read small print and watch television. Through the support of the California Institute for Regenerative Medicine, I’ve also developed a novel minimally invasive stem cell-based treatment, CPCB-RPE1, for patients with an advanced form of dry AMD, which is in a Phase I/IIa clinical trial. The implanted scaffold of RPE are localized, and can function to support and replenish dying photoreceptors of the retina, which would help restore and prevent vision loss in patients with AMD.” Mark Humayun, Cornelius J. Pings Chair in Biomedical Sciences, Professor of Ophthalmology, Biomedical Engineering, and Integrative Anatomical Sciences; Director, USC Institute for Biomedical Therapeutics; Co-Director, USC Roski Eye Institute at the University of Southern California, Los Angeles, CA, USA.
“Once we have regulatory approval for [Nightstar’s] gene therapy programs for recessive diseases, we will need to look at other technologies for dominant diseases and we have exciting CRISPR projects in the pipeline.” Robert MacLaren, Professor of Ophthalmology at the University of Oxford, UK; and Founder of Nightstar.
“[The future?] Improved recovery of vision after retinal detachment repair, gene therapy and stem cell treatments.” Stanley Chang, Former Edward S. Harkness Professor and Chairman of the Department of Ophthalmology and K.K. Tse and Ku Teh Ying Professor of Ophthalmology, Columbia University Medical Center, New York Presbyterian, New York, NY, USA.
“[Exciting developments?] The increasing awareness of the importance of neural cell health and not just the amelioration of exudative manifestations of AMD and diabetes, as well as the consideration of combined therapies to reduce neural cell loss.” Usha Chakravarthy, Professor, Ophthalmology and Vision Sciences, Royal Victoria Hospital (The Belfast Trust) and Queens University of Belfast, Northern Ireland.
Outside the OR…
“I believe that healthcare will be transformed in the next 10 years by the introduction of AI, in particular a technique known as “deep learning”. I would like ophthalmology to be the medical specialty leading the way in this regard (and I would like my institution, Moorfields Eye Hospital, to be playing a key role in this). In the short term, I believe that AI will greatly increase our knowledge of ophthalmic disease using imaging techniques that are already widely available. In the longer term, I think there will be much closer integration between imaging data and omics data – ‘AI-assisted science’ will be required to facilitate this.” Pearse Keane, Consultant Ophthalmologist, Moorfields Eye Hospital, London; NIHR Clinician Scientist at Institute of Ophthalmology, University College London, UK.