PTA Is Not the Way
We need to rethink the concept of PTA as a predictor of post-LASIK iatrogenic ectasia risk
Percent tissue altered (PTA) has been presented as a significant predictor of post-LASIK ectasia risk (1)(2). But I don’t believe that it is – and I’d like to explain why.
There are two major drawbacks that limit the applicability of PTA in our daily practice. Firstly, the way PTA has been computed does not reflect the true biomechanical instability induced by LASIK. Secondly, a risk factor should not be used as a screening metric.
1) The core limitation of PTA:
In their 2014 preliminary paper, Santhiago et al. (1) achieved 97 percent sensitivity and 89 percent specificity for PTA ≥40 as a predictor for ectasia in post-LASIK patients who had normal pre-operative topography. But there was no external validation of these findings until recently. We have made it our objective to evaluate the PTA metric in independent patient populations. We first performed a retrospective analysis of 593 eyes with normal pre-operative topography that underwent LASIK surgery and had a minimum of two years follow up (3). Not a single case of iatrogenic ectasia was found – despite 126 eyes (21 percent) having a PTA ≥40, and with 19 eyes (3.2 percent) having a PTA >47 – a value which Santhiago et al. (1) reported as having 100 percent specificity. Thus, our independent study did not confirm the specificity of PTA as a predictor for ectasia. In fact, the 126 cases would have been unnecessarily rejected for LASIK surgery if PTA>40 was applied as a screening tool in this population. A recent study by Djodeyre et al found similar results with 20 percent of their cases having a PTA>40 and none developing iatrogenic ectasia (4).
We then sought to determine if PTA>40 was able to detect cases that developed iatrogenic ectasia. For that purpose, we performed a multi-center study (involving Fondation Ophtalmologique Rothschild, Centre D’Ophtalmologie, and Clinique Lamartine, Paris, France; Singapore National Eye Centre and Eye Surgeons at Novena, Singapore; Gavin Herbert Eye Institute, Irvine, California, and Pepose Vision Institute, Chesterfield, USA; Departement d’Ophtalmologie, Universite de Montreal, Canada; Narayana Nethralaya Hospital, Bangalore, India; Asian Eye Institute, Manila, Philippines; and London Vision Clinic, London, UK; data under review). Together, we identified 23 eyes with normal pre-operative topography that developed iatrogenic ectasia after LASIK surgery, and compared their PTA with 80 unaffected eyes. PTA>40 was present in only 11 of the 23 cases (sensitivity = 47.8 percent) and 12 iatrogenic ectasia cases had a PTA<40. Groden et al. (5) also recently reported a very low sensitivity of PTA for predicting iatrogenic ectasia (15 percent).
Our patient populations have not been able to validate the utility of PTA. In fact, our studies have shown that PTA is not a reliable analyzer of the true biomechanical instability induced by LASIK surgery. One possible explanation is that when calculating PTA, the cornea is being considered in only two dimensions. PTA assumes that all flaps will have the same diameter and optical zone. When a flap is created with the same planned thickness but a larger diameter, a higher amount of biomechanical instability may be induced, but the PTA value remains the same. In addition, when you go from a 5 mm to a 7 mm optical zone, the volume ablated increases by three-and-half times even though ablation depth only increases by 1.5. All this is not taken into account in the PTA calculation, limiting its benefits.
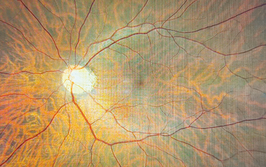
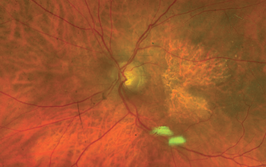
In addition, the study performed by Santhiago et al. was based only on Placido disc topography, despite the fact that there are clearly reported advantages of using both topography and tomography to detect very early stage of keratoconus (KC) (6–8). Thus, it’s difficult to ascertain if some of the patients classified as “normal” based on Placido topography in the PTA study are not in fact “subclinical KC” if tomography was used to classify them. The subclinical KC status would explain why a threshold lower than 40 would be required for PTA to correctly predict ectasia risk in such cases.
2) A risk factor should not be used as a screening tool.
PTA>40 as a risk factor for ectasia was conceived from data derived from a single population. Confirmation of the validity of PTA has not been achieved in external groups, yet it has been commonly advocated to use PTA>40 as a screening tool for refractive surgery candidates and to exclude patients with PTA>40 from LASIK. Different studies (9)(10) have shown how strongly a risk factor needs to be associated with a disease before it is likely to be a useful screening test. Based on those studies and our data, PTA would barely yield a detection rate of 40 percent, limiting its use and benefits as a screening tool.
I applaud the good work done by Marcony Santhiago and his colleagues in trying to identify new risk factors for iatrogenic ectasia and decreasing LASIK complications. However this concept has not been elucidated effectively and pushing it forwards to be used as a screening tool is detrimental as a whole to refractive surgery.
In future, in order to decrease ectasia risk, we should focus on improving the pre-operative screening of patients by involving both tomographic and topographic assessments rather than Placido disc analysis alone (as done in the PTA study) to identify eyes with early KC. In addition, exploring the concept of percent of volume altered as a risk factor, which thus evaluates the cornea in three dimensions, would be more logical and relevant.
The PTA preliminary results have not been reproducible nor validated in external groups. PTA is not the whole story – there is certainly more to consider.
Special thanks to Damien Gatinel, Cordelia Chan, and Perry Binder for their help in this work.
- MR Santhiago et al., “Association between the percent tissue altered and post-laser in situ keratomileusis ectasia in eyes with normal preoperative topography”, Am J Ophthalmol, 158, 87–95 (2014). PMID: 24727263.
- MR Santhiago et al., “Role of percent tissue altered on ectasia after LASIK in eyes with suspicious topography”, J Refract Surg, 31, 258–265 (2015). PMID: 25884581.
- A Saad et al., “Evaluation of the percentage tissue altered as a risk factor for developing post-laser in situ keratomileusis ectasia”, J Cataract Refract Surg, 43, 946–951 (2017). PMID: 28823442.
- MR Djodeyre et al., “Long-term evaluation of eyes with central corneal thickness <400 µm following laser in situ keratomileusis”, Clin Ophthalmol, 10, 535–540 (2016). PMID: 27099459.
- LR Groden et al. “Percentage tissue altered in a large series of post-femtosecond LASIK ectasia cases”. Presentation at the American Society of Cataract and Refractive Surgeons annual meeting; Los Angeles, California; May 5–9, 2017.
- IC Ramos et al., “Variability of subjective classifications of corneal topography maps from LASIK candidates”, J Refract Surg, 29, 770–775 (2013). PMID: 23980708.
- R Ambrósio Jr et al., “Novel pachymetric parameters based on corneal tomography for diagnosing keratoconus”, J Refract Surg, 27, 753–758 (2011). PMID: 21800785.
- A Saad and D Gatinel. “Topographic and tomographic properties of forme fruste keratoconus”, Invest Ophthalmol Vis Sci, 51, 5546–5555 (2010). PMID: 20554609.
- C Chan et al., “Validation of an objective scoring system for forme fruste keratoconus detection and post-LASIK ectasia risk assessment in Asian eyes”, Cornea, 34, 996–1004 (2015). PMID: 26165793.
- N J Wald, A K Hackshaw, C D Frost. When can a risk factor be used as a worthwhile screening test? BMJ 1999;319:1565–8
Alain Saad is a refractive surgeon in Damien Gatinel’s Department, Rothschild Foundation, Paris, France, and Assistant Professor at the American University of Beirut, Lebanon.