The Eye Exam's Quantum Leap
A future of skyrocketing patient numbers in the clinic and technological advances means that the routine eye exam of tomorrow has to be substantially different. But how?

For over 100 years, the slit lamp has been a fundamental unit of the eye exam. But since Alvar Gullstrand described its precursor in 1911, the technology has barely changed at all. With the global elderly population predicted to double between now and 2040, and the number of ophthalmologists being trained each year remaining largely static, the burden on already heavily oversubscribed eye clinics is only going to increase. Almost every patient that presents to an ophthalmologist will receive an eye exam – and as such, the number of these exams is going to skyrocket too. Is the humble slit lamp up to the challenge? We think not. It’s time the eye exam was rethought and recreated in order to keep up with the challenges ophthalmologists face today – and will face tomorrow. We believe that the solution lies in a technology already well established in ocular imaging: optical coherence tomography (OCT).
OCT: better, but not enough
OCT has revolutionized the diagnosis and treatment of ophthalmic disease, and retinal disease in particular. It provides cross-sectional images of the retina with extremely high axial resolution. It does this so effectively, that it’s sometimes referred to as in vivo clinical biopsy. But more than that, it owes its dominance at least in part to how safe, quick and easy it is to perform, and how well-tolerated it is by patients. So we can easily obtain an OCT scan for both the elderly and children – in fact, it’s often easier to acquire an OCT scan from a child than it is to actually examine them with a slit lamp
or ophthalmoscope.
Moorfields Eye Hospital regularly audits the number of OCT scans that are performed, and in the last week of April 2015, this number was more than 2,500. That’s a number that is set to rapidly increase for the foreseeable future. In a few years’ time, this could quite feasibly double to 5,000 OCT scans per week, and in the future it would not be surprising if every patient who arrives for an eye examination has a visual acuity (VA) measurement and an OCT exam, even if retinal disease isn’t suspected.
But OCT today isn’t perfect; it has limitations. One issue is the size of the devices. Although they are smaller than CT or MRI scanners, they’re large nonetheless. Another is the need for a photographer or trained healthcare worker to acquire the images. Another crucial restriction is the depth range of OCT. For example, one common OCT instrument, Heidelberg Engineering’s Spectralis, has a depth range of 1.9 mm. This is perfect for capturing the retina, which is approximately a quarter of a millimeter in thickness, but a serious limitation when it comes to imaging other structures in the eye.
But this is changing – in recent years we’ve seen the development of new swept-source laser light sources for OCT that have greatly expanded the depth range of current conventional devices. For example, we now have vertical cavity surface emission (VCSEL) lasers, which have a depth range of between 40 and 60 mm – a massive improvement from 1.9 mm. This provides the potential to scan the whole eye; a typical eye has an axial length of around 20–25 mm. Which leads us to our concept – binocular OCT.
Taking Binocular OCT from Theory to Reality
- Binocular OCT is the brainchild of Alexander Walsh, an ophthalmologist and mechanical engineer trained at Stanford University.
- Envision Diagnostics is the company founded by Alexander to develop and commercialize the device, with an aim of eventually making it available to clinics and to patients, potentially in their own homes.
- The team now plan to create a prototype of the device at Moorfields Eye Hospital and begin clinical testing and validation.
- Pearse Keane, based at Moorfields Eye Hospital, will be working to assess the accuracy, reliability and reproducibility of the device, funded by a National Institute of Health Research (NIHR) Clinician Scientist award.
- Initially, the device will be studied in patients with age-related macular degeneration, and it is hoped that subsequent studies may look at glaucoma, pediatric patients, and neurological diseases.
Box 1. Taking the idea, commercializing it, next steps, and plans for the future.
A binocular vision
Binocular OCT is being developed in Los Angeles by the company Envision Diagnostics (see Box 1), a startup aiming to create a commercially available device. There are three reasons why we believe binocular OCT is far more exciting than simply a device for providing structural imaging of the eye. Firstly, the fact that it is binocular in nature means that the user will be able to align the optical axis of the device with their optical axis – allowing them to scan their own eyes without the need for a photographer or healthcare assistant (see Figure 1).

Figure 1. A 3-D render of the proposed hand-held binocular OCT device.
Secondly, the device is smart – the screens on the device will mimic smartphone or tablet computer screens that can display a wide variety of content to the user (see Figure 2). For example, the device could play a cartoon while at the same time using invisible light to make measurements of the eyes’ function.
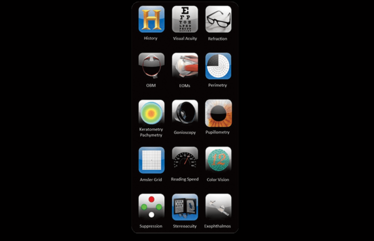
Figure 2. The smartphone-like interface of the binocular OCT that users could interact with.
Finally, it’s simultaneous, imaging both eyes at once. This means a range of additional diagnostic testing can be performed, such as VA measurements, pupil measurements, visual field tests, refraction, and extraocular movements – many of the tests that a slit lamp, dilated fundus exam, or healthcare professional can perform (see Table 1).

Table 1. The potential capabilities of binocular OCT in comparison to other types of ocular examination. ✓/X denotes examinations which could be carried out, but would potentially be challenging, or only partial.
Improving workflows and waiting times
We believe that the way we carry out eye exams needs to change, and soon, because the needs of our patients are changing. We have entered an era where effective treatments for many of the common causes of blindness exist, but a huge burden remains on patients, as they must attend regular eye clinics for extended periods of time. For example, if they are receiving anti-VEGF treatments, they may have to come in every four to six weeks to see whether they need another injection – potentially for years at a time. And these patients commonly wait two to three hours, often for relatively straightforward appointments. Of course, part of the reason for these delays is related to the huge volumes of patients many eye hospitals must now deal with. But it’s also partly caused by the inefficient workflows in most, if not all, eye clinics (see Figure 3).
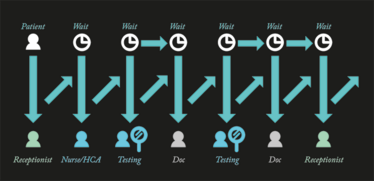
Figure 3. A typical workflow for a patient visiting an eye hospital for a routine appointment.
A typical workflow looks something like this: the patient arrives, and must wait for the receptionist. Then they need to wait for the nurse to call them and measure their VA, and give them their eyedrops. Then they have to wait for an OCT scan to be performed, and then wait for the doctor to call them in. Then, their doctor might decide they didn’t get the OCT scan they wanted and send them for another one – then they wait some more for the scan and then wait to see the doctor again. And even once their appointment is over, they may once again have to wait to see the receptionist to make their next appointment. We’ve used the word “wait” seven times in the last two sentences describing the process, so it’s no surprise that this is a significant burden for our patients, who often wait many, many hours to have their chronic eye conditions treated.
There’s also the societal burden to consider too: hospital resources cost money, and patients and carers aren’t being economically productive while they are travelling to and from the hospital and waiting hours for routine, straightforward, short appointments. Efficiencies would save everyone both time
and money.
Standardization and automation
Many of these hours could be saved by automation. The American philosopher Eric Hoffer said, “When you automate an industry, you modernize it.” You could use various examples for this, but the one that stands out is banking. In the 1970s or 1980s, if you wanted to take out even a small amount of money, you had to go and queue up. For the last 20 years, we have performed most of our interactions with the bank at an ATM or over the telephone, and the last decade has seen many of these functions being performed online.
What if we could create a similar streamlined way to have eye exams? A prototype of our device, for example, is able to automatically measure VA – the patient sees letters of different sizes when looking into the machine, and responds to what they see. Voice recognition is used to compare their responses to the correct answers, and then the information is conveyed wirelessly to a tablet computer. See video below.
Figure 4. A binocular OCT automated eye exam.
Another area that could be greatly improved is quantitative analysis – for example, take handwritten doctors’ notes. They can be very subjective, and convey very little information. Further, sometimes handwriting can be virtually illegible, and consequently hard to understand. When you look at some doctors‘ notes (Figure 5), it is perhaps unsurprising that sometimes subtle changes in disease are not picked up over time – particularly in the context of public healthcare systems such as the National Health Service, where a patient may see a different doctor every time they have an appointment. We believe this sort of record keeping needs to be left behind. As we transition to an era of medical care dominated by digital data, eye care providers need more objective, reproducible and quantitative analyses for every aspect of the eye exam.
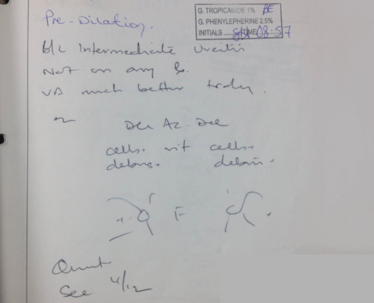
Figure 5. Illegible handwriting in patient notes can make subtle changes to their eyes hard to spot.
Take pupillometry – we shine a pen torch into the eye and produce a fairly subjective and inaccurate measurement, but using binocular OCT, the pupils could be measured accurately and quantitatively with imaging of the anterior segment (see Video below), generating data such as the maximum and minimum diameter of the pupil, the percentage of afferent pupillary defect, or other information such as velocity, acceleration, latency, and so on (see Figure 7).
Figure 6. Measuring the pupil using binocular OCT.
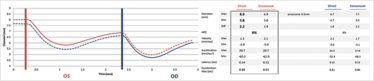
Figure 7. An example of the data binocular OCT can generate from a pupil examination.
Another example is extraocular movement – using binocular OCT, the patient looks at the screen and follows a fixation cross with their eyes. We can use eye tracking to see how the eye is moving based on the tilt of the anterior segment (see Video below). These data can be measured, stored for perpetuity and compared to previous measurements or normative databases.
Figure 8. Using binocular OCT, the patient looks at the screen and follows a cross with their eyes, and eye tracking can be used to see how the eye is moving, using the rotation of the anterior segment.
We believe our method could provide a wealth of quantitative information that is currently “left on the table” using standard methods. By comparing results from these tests to age-gender- and race-matched normative data, we believe that eye care providers will be able to detect subtle changes that might otherwise go undetected. By placing all of these measurements in a single, digital dataset, we believe that portability, storage and interchange of eye examination data can be vastly improved. And by encompassing all of these tests in a single device, we hope that we can standardize the eye examination around the world so that eye diseases in London, Kiribati can one day be diagnosed with the same ease as eye diseases in London, England.
From prototype to home test?
We believe binocular OCT has a host of potential benefits, and could soon become the go-to method for quick and easy eye examination. We are now in the process of testing and validating our prototype device, and hope to gain a CE mark by 2018. Although OCT devices are generally class I lasers that are quite safe to use in most conditions, they typically require special controls to minimize the risk to the patient. Fortunately, since OCT is already such a well-established and well-accepted imaging modality, it is our hope that regulatory approval will not be a significant hurdle.
Our prototype will initially be able to perform around five or six different tests, but in the future, 50 or more different diagnostic tests could be incorporated. It’s possible that these devices could be manufactured cheaply, and they might eventually reach a consumer level of affordability – consider a future where patients take tests in pharmacies, shopping malls, or even in their own homes! Such a cheap and portable device would also have obvious applications in the developing world.
Although binocular OCT is still in the early stages of development, the advent of sophisticated, extended-depth OCT and the unmet clinical need for faster, easier and more reliable eye exams makes this the perfect time to give the eye exam an overhaul. We hope that our device could soon be used to reduce costs and increase efficiency for hospital eye services, but more importantly, it might allow us to improve the quality of patient care through much better quantitative analysis of the eye.
Pearse Keane is a consultant ophthalmologist at Moorfields Eye Hospital, London, an acknowledged world expert in OCT imaging, and the first ophthalmologist in the UK to receive an NIHR Clinician Scientist Award.
Alex Walsh is the founder and chief executive of Envision Diagnostics Inc., based in Los Angeles, California. He is also a board certified ophthalmologist, based at Retina Vitreous Associates Medical Group, Los Angeles.
A specialist in in applied clinical imaging research, Pearse has a particular interest in optical coherence tomography. Now a consultant at Moorfields Eye Hospital, he previously carried out OCT research with some of the original inventors of the technology at the Doheny Eye Institute. As the first UK ophthalmologist to receive a Clinician Scientist Award from the National Institute of Health Research, his current work focuses on exploring the potential of new technologies and innovations in the treatment of visual impairment and blindness.
Alex, an engineer and a board-certified ophthalmologist based at Retina Vitreous Associates Medical Group, USA, is best known for binocular OCT – an idea he first formulated while at the Doheny Eye Institute. He is now the founder and chief executive of Envision Diagnostics Inc., a medical device company developing specialized ophthalmic imaging tools. With his degrees in both engineering and medicine, he’s well-placed to solve tricky diagnostic problems, and his plethora of patents and peer-reviewed journal articles bear this out.